The all-natural, drug-free lung expansion and mucus clearing device. Used in hospitals worldwide – now available in your pocket.
The all-natural, drug-free lung expansion and mucus relief device. Used in hospitals worldwide – now available in your pocket.
The all-natural, drug-free lung expansion and mucus relief device. Used in hospitals worldwide – now available in your pocket.









We’re backed by science – and approved by the best. Learn more about the innovation driving Turboforte and our incredible results.

Registered by the Australian Governments Therapeutic Goods Association (TGA).

Turboforte meets the European Union's (EU) standards for health, safety, and environmental protection.
Using the latest in medical innovation, we’ve created an answer for clearer, healthier and stronger lungs – all in one small but powerful package.
The all-natural, drug-free lung expansion and mucus relief device. Used in hospitals worldwide – now available in your pocket.

Using the latest in medical innovation, we’ve created n answer for clearer, healthier and stronger lungs – all in one small but powerful package.
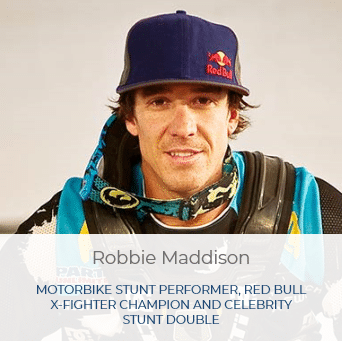
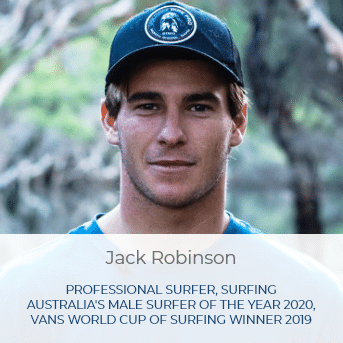
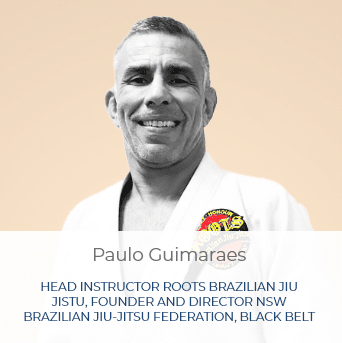
From the world’s most elite athletes, talented and aspiring musicians, those suffering from respiratory illnesses and those who care for them, Turboforte has helped increase lung capacity for thousands of customers.


We’ve helped thousands of people increase their lung capacity. Don’t just take our word for it.












From the athlete wanting more performance, to the musician after increased lung capacity, all the way to patients after medical relief, Turboforte prevents the impact of pollution on the respiratory system.

Turboforte alleviates the
symptoms of lung and respiratory conditions including:
Get the competitive edge with our all-natural solution, increasing your lung capacity for sports like:

Clear airways and greater lung capacity for diaphragmatic breathing, helping you be a better:
Turboforte is a handheld, drug-free device that’s safe for everyday use, making it suitable for:
Turboforte Lung Physio is a handheld, drug-free, lung expansion, breathing exerciser & mucus clearing device that helps clear congestion from airways and lungs making breathing easier.

USD $49.95
Turboforte Lung Physio is a handheld, drug-free, lung expansion, breathing exerciser & mucus clearing device that helps clear congestion from airways and lungs making breathing easier.

USD $49.95